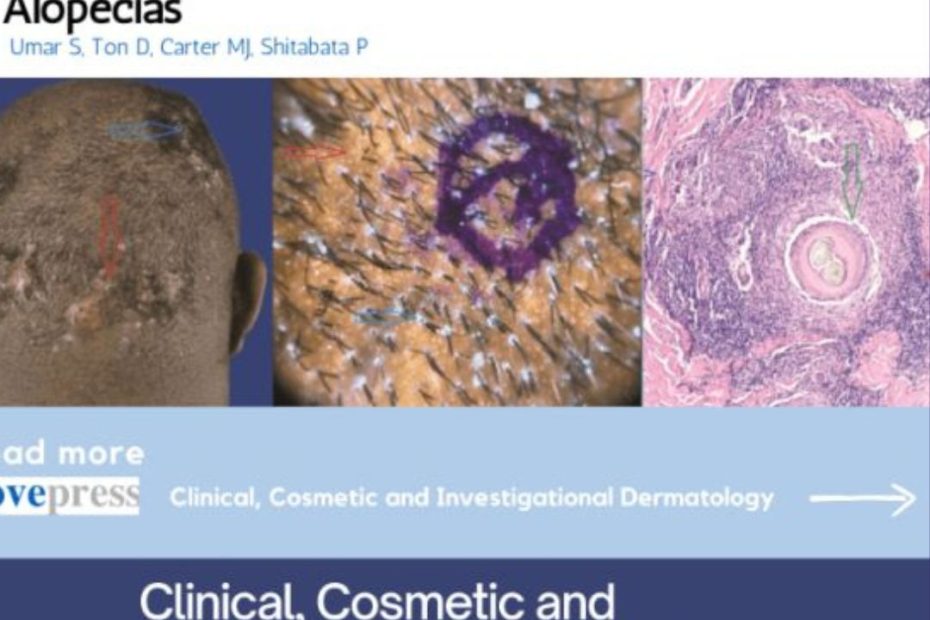
What is PIILIF?
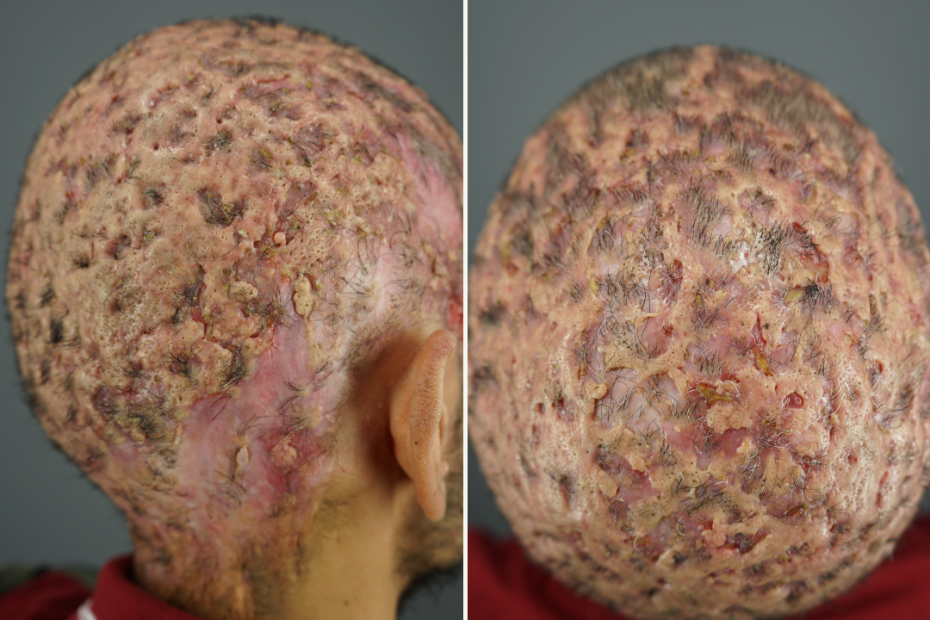
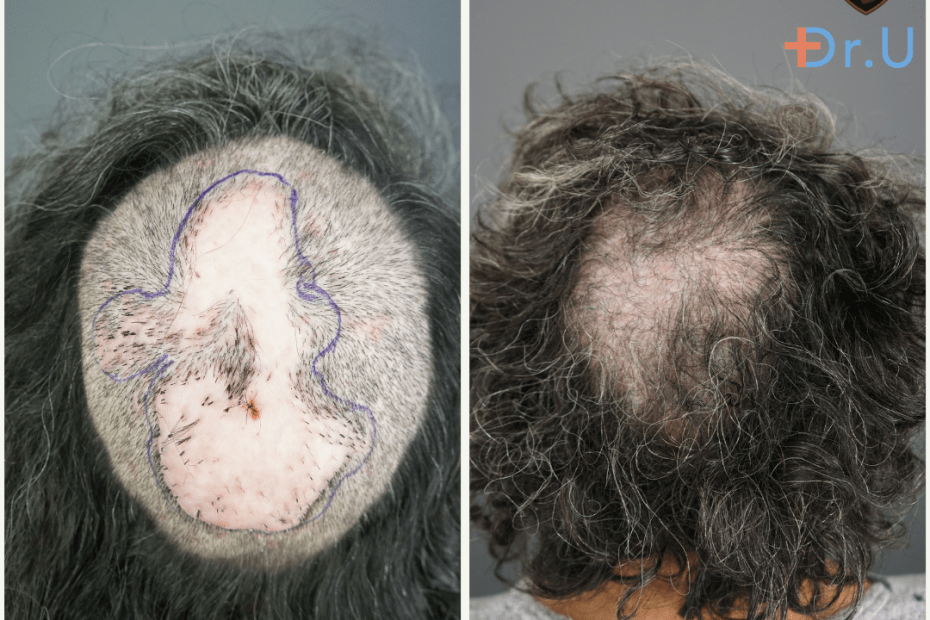
What is PIILIF (Perifollicular Infundibulo-Isthmic Lymphocytoplasmic Infiltrates and Fibrosis)? It is a dermatological condition characterized by inflammation of hair follicles, hair loss, and scalp scarring.… Read More »What is PIILIF?