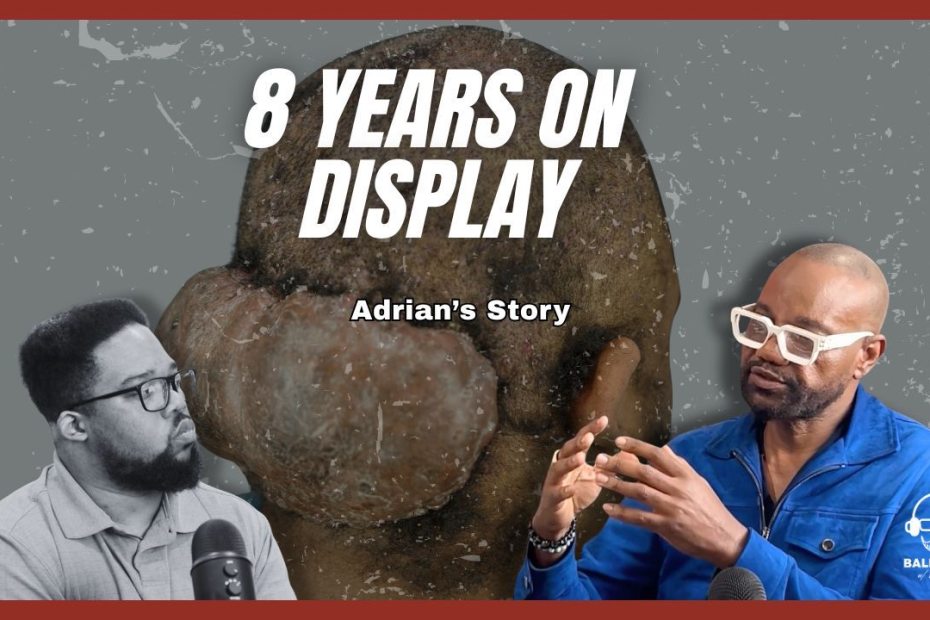
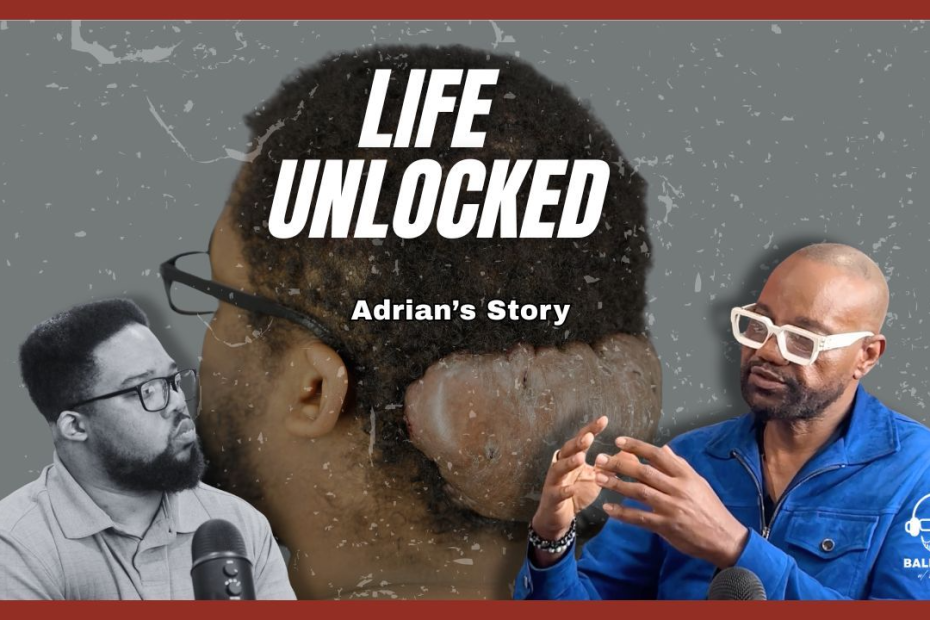
When Medicine Misses: Adrian’s Dreams on Hold
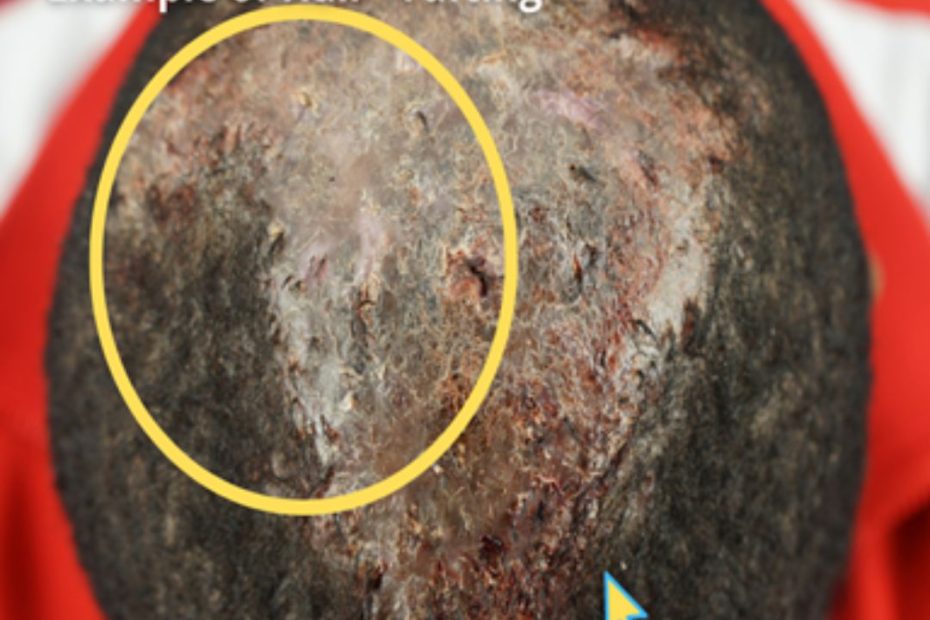
For eight years, Adrian did everything he could to help himself. He rotated through clinics and tried first-line therapies for Acne Keloidalis Nuchae, like corticosteroids,… Read More »When Medicine Misses: Adrian’s Dreams on Hold