Do You Want to Get a Permanent Solution to Your Folliculitis Decalvans (FD) Condition?
Folliculitis Decalvans (FD) is a form of scarring Alopecia that is difficult to treat and manage. Current treatment options used to manage FD often offer temporary solutions.
A Smarter and Better Surgery for Folliculitis Decalvans
There is a way to permanently eliminate folliculitis decalvans. Four men and a woman suffering from the condition received treatment by surgically removing lesions from the affected areas.
The methods include:
- Surgical excision
- Second-intention healing
Surgical Excision and Second-Intention Healing
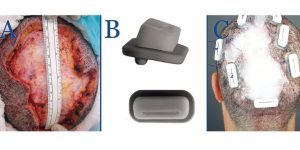
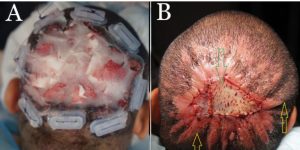
A recent Clinical Cosmetic and Investigative Dermatology study described a novel procedure for treating Folliculitis Decalvans. This technique involved a specialized method of excising the lesions and applying patented Athena Suture Kits to facilitate wound closure. The authors observed that this method effectively and permanently eliminated Folliculitis Decalvans. Notably, the approach successfully employed second-intention wound healing on typically convex surfaces, a departure from its usual application on concave terrains.
Success Stories Published in a Medical Peer-Reviewed Study
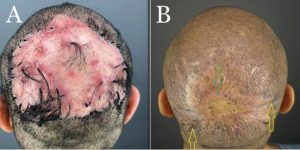
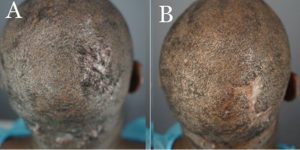
Dr. Sanusi Umar, a pioneer in the field, became the first to perform the surgical excision of Folliculitis Decalvans (FD), a chronic and challenging scalp condition. This groundbreaking procedure was highlighted in a peer-reviewed medical study where five patients with varying severities of FD underwent surgery to remove their FD lesions.
According to the Clinical Cosmetic and Investigative Dermatology publication, these patients had previously tried other treatment methods without success. The thickness of their FD lesions made them unsuitable candidates for alternative treatments like laser therapy, radiation, and other conventional approaches.
The medical publication also highlighted that within 18 months, Dr. Umar successfully performed all five surgeries at his Los Angeles clinic, permanently eliminating the FD condition.
Dr. Umar, AKA Dr. Bumpinator, utilizes a meticulous excision procedure for FD lesions with minimal tissue damage. He also uses Guarded High-Tension Sutures to guide wound contraction, ensuring optimal healing and reducing the risk of recurrence.
Skin Grafting
After lesion excision, wounds that do not close and exceed a certain diameter length due to the surgical process will require skin grafting.
Below are Real-Life Patient Photos and Videos



VIDEO: Folliculitis Decalvans Surgical Excision Before and After
Patient Selection Criteria Developed by Dr. Bumpinator
Dr. Sanusi Umar, known for his innovative approach to treating Folliculitis Decalvans (FD), credits his success to careful patient diagnosis and selection of appropriate treatment methods.
FD presents with varying lesion sizes and affects different areas of the scalp, meaning that a single treatment approach may not be practical for all patients. Recognizing this, Dr. Umar has developed tailored treatment plans.
By customizing treatment according to the extent and location of FD lesions, Dr. Umar ensures that each patient receives the most effective care, giving better results.

What Does Folliculitis Decalvans Look Like?
FD occurs as a result of inflamed hair follicles. Trapped bacteria causes acne-like red and pus-filled lesions on the affected areas, leading to pain and itchiness.
Who Gets Folliculitis Decalvans?
Folliculitis Decalvans can affect both men and women. In addition, there are higher incidences of FD in people of color. Learn more about Folliculitis Decalvans here.
If you are struggling with Folliculitis Decalvans and want to speak to Dr.Bumpinator, click the free consultation button below to get started.
References
Umar, Sanusi, et al. “Refractory Folliculitis Decalvans Treatment Success with a Novel Surgical Excision Approach Using Guarded High-Tension Sutures.” Clinical, Cosmetic and Investigational Dermatology, vol. Volume 16, 1 Sept. 2023, pp. 2381–2390, https://doi.org/10.2147/ccid.s422077.
Also Read
https://bumpinator.com/ear-keloid-treatment-that-youll-be-happy-with-permanently/
https://bumpinator.com/bumpinator/what-is-folliculitis-decalvans/